ComfortPro
Premium Probiotic Formula...
Key Ingredients

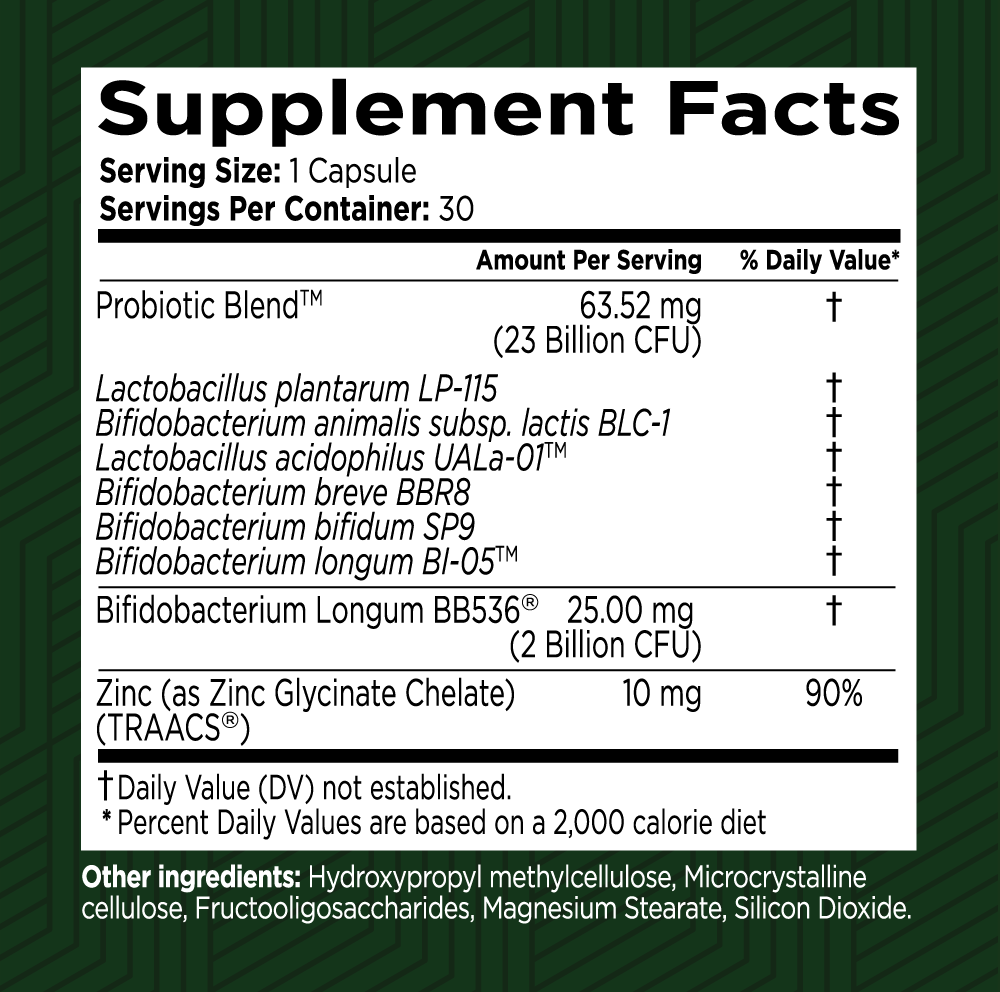
Zinc (as Zinc Bisglycinate chelate) (TRAACS")
A special form of zinc called Zinc Bisglycinate Chelate in ComfortPro is included for its role in supporting healthy colon walls and improving overall digestive health. Strengthens colon walls. Enhances zinc absorption. Supports immune health. Aids digestive enzyme production. Addresses zinc deficiencies in older adults.

Bifidobacterium longum BB536°
Bifidobacterium longum BB536® is a revolutionary "Bioidentical Probiotic" and is recognized as the world’s first probiotic strain that perfectly matches the same strain naturally present in the human gut from birth. This unique probiotic is designed to restore healthy digestion and promote regular bowel movements. Here’s a detailed description of its benefits and functions.

Probiotic Blend
The Probiotic Blend, featuring Lactobacillus acidophilus UALa-01™, Bifidobacterium lactis UABla-12™, Lactobacillus plantarum UALp-05™, Bifidobacterium breve UABbr-11™, Bifidobacterium bifidum UABb-10™, and Bifidobacterium longum UABI-14™, is a potent combination designed to support optimal digestive health and overall well-being. Here’s a detailed description of its benefits and functions.
Frequently Asked Questions
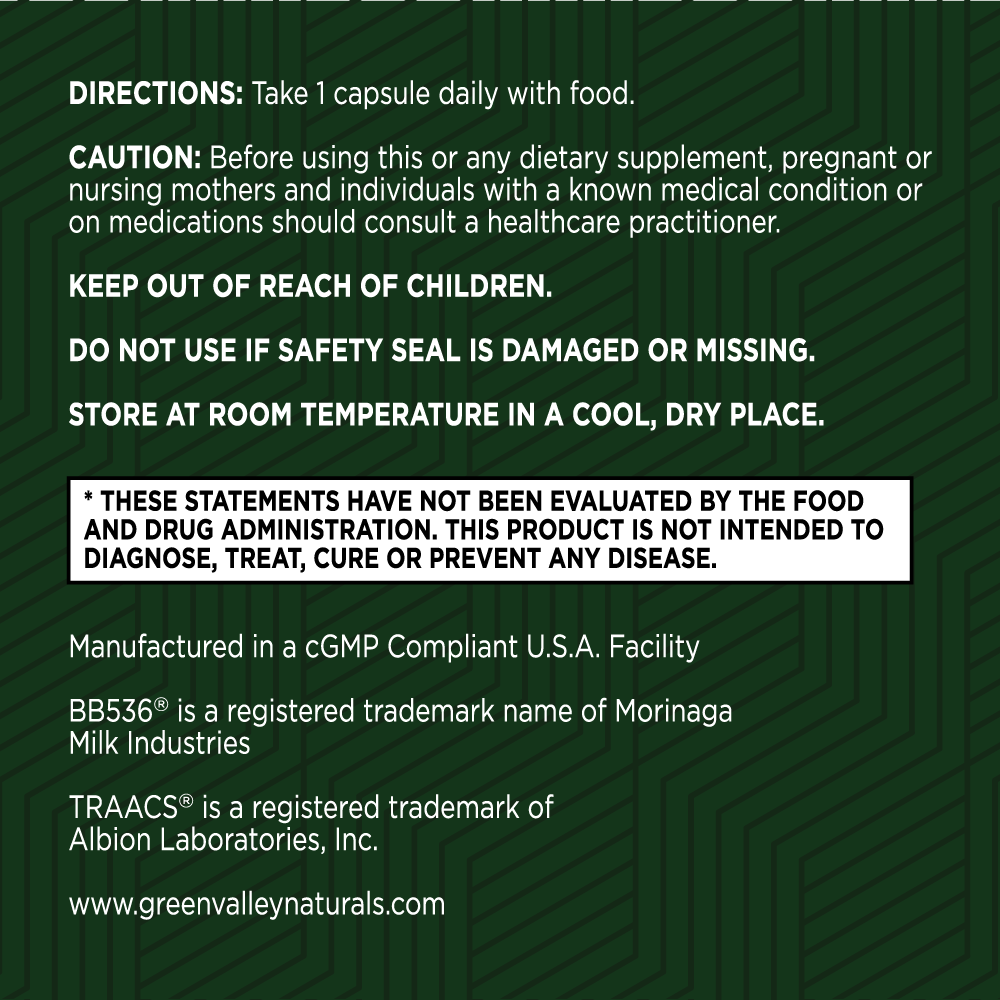
Your health is our top priority
Here at Green Valley, we only work with US-based manufacturing facilities that are cGMP (Good Manufacturing Practices) compliant and FDA inspected.
Our products are triple tested by our manufacturers to ensure potency and purity and are stored in our temperature and humidity-controlled warehouse right here in the Shenandoah Valley, Virginia. And we ship directly to your doorstep – we don’t share warehouse space and we don’t hand off your business to a third party to fulfill your order.
Best of all, all Green Valley products come with our 90-day Satisfaction Guarantee. If you are unhappy with the product for any reason, simply call or email our customer support team and return the unused portion of the product within 90 days of your order. We’ll refund every penny of your purchase (less shipping), no questions asked!

ComfortPro Customer Reviews
Green Valley Natural Solutions has excellent products and offers excellent service! Orders are promptly adjusted and filled upon request
Green Valley Natural Solutions has excellent products and offers excellent service! Orders are promptly adjusted and filled upon request. Delivery is quick and reliable. Great folks!
Fine, excellent customer service
Fine, excellent customer service. Along with fine, excellent supplemental products, likewise!!
I am using ComfortPro probiotics and so far so good
I am using ComfortPro probiotics and so far so good. I feel my gut is starting to do what it is supposed to do. The uncomfortableness I used to feel as at a minimum. I recommend this product. I have IBS and gut issues. Waiting to see what the future holds.