My Sinus Miracle
Safe Herbal Relief...
Key Ingredients

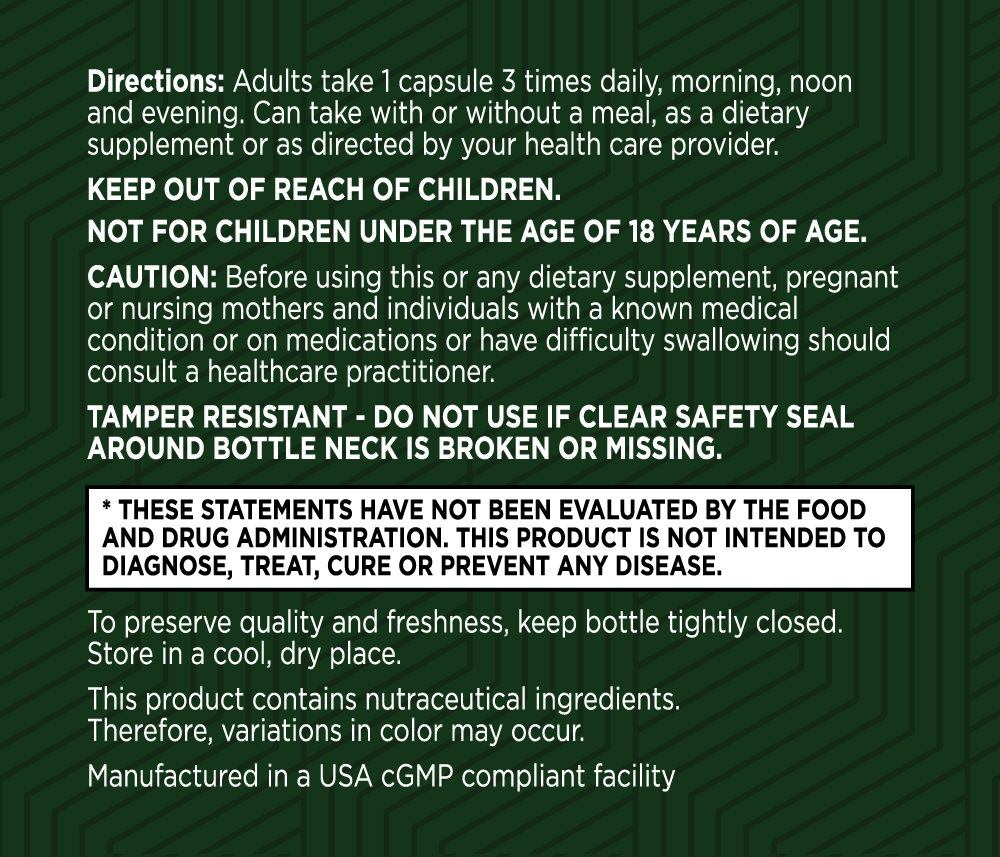
Pelargonium Sidoides Root Extract (30:1) (18 mg equivalent to 540mg of dried Pelargonium Sidoides Root Powder)
Derived from the South African geranium, this extract is used to bolster the immune system. It's believed to help block nasal irritants from invading cells and to increase ciliary beat frequency, aiding in the movement of mucus out of the sinuses for better drainage and relief.

Elderberry Fruit Extract 10:1 (10% Anthocyanins) (Sambucus nigra L 14 mg equivalent to 140 mg Elderberry Fruit Powder)
Known for its immune-supporting properties, elderberry is included to help the body resist and fight off respiratory irritants. It contains proteins that block irritants from entering cells.

Quercetin Dihydrate (Sophora Japonica L) (Flower)
A flavonoid found in fruits and vegetables, quercetin is included for its ability to support a healthy inflammatory response. It helps stabilize immune cells (mast cells) to reduce the production of histamine, thereby lessening sinus discomfort and swelling.

N-Acetyl-L-Cysteine
This amino acid is used to promote a healthy inflammatory response in the sinuses. NAC is known to dissolve mucus, making it less thick and sticky, which aids in clearing sinus passages.
Vitamin D3 (as cholecalciferol)
Vitamin D3 (as cholecalciferol) is a vital nutrient for maintaining bone health, supporting immune function, and promoting overall wellness. Its ability to enhance calcium absorption, modulate the immune system, and reduce inflammation makes it an essential ingredient for those seeking to improve their respiratory health and overall quality of life.
Frequently Asked Questions
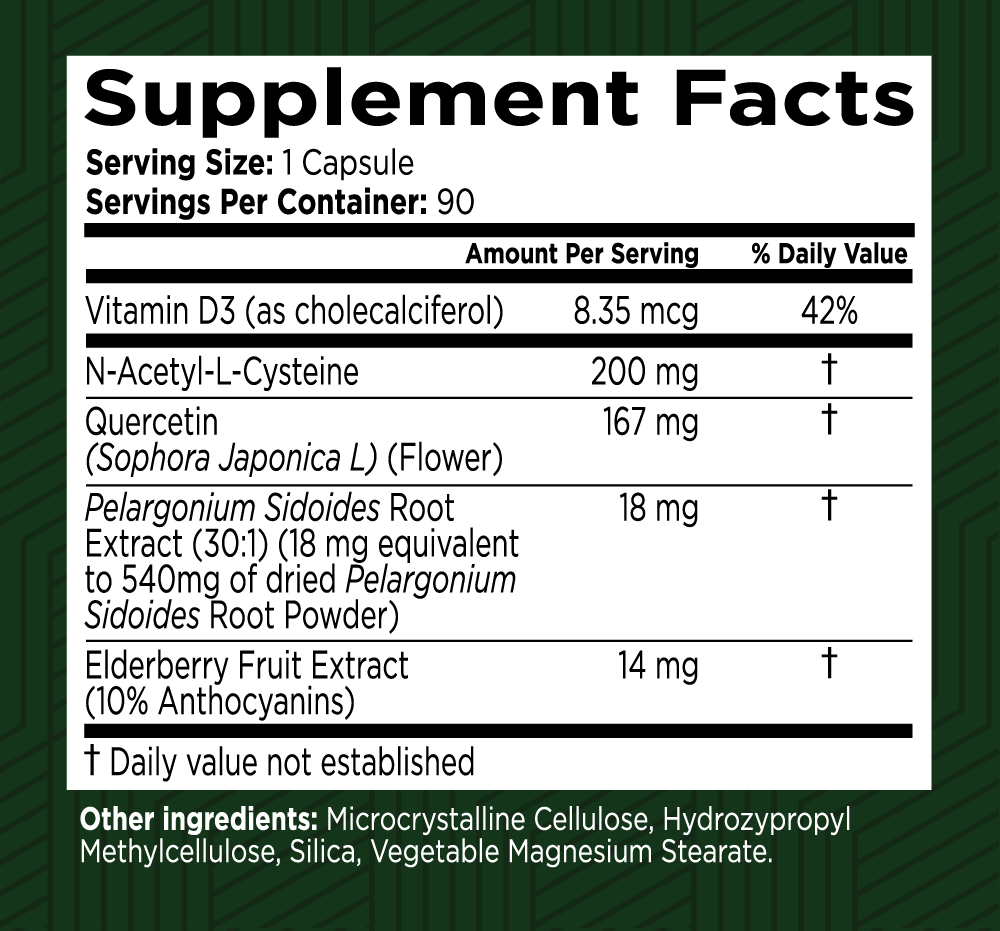
Your health is our top priority
Here at Green Valley, we only work with US-based manufacturing facilities that are cGMP (Good Manufacturing Practices) compliant and FDA inspected.
Our products are triple tested by our manufacturers to ensure potency and purity and are stored in our temperature and humidity-controlled warehouse right here in the Shenandoah Valley, Virginia. And we ship directly to your doorstep – we don’t share warehouse space and we don’t hand off your business to a third party to fulfill your order.
Best of all, all Green Valley products come with our 90-day Satisfaction Guarantee. If you are unhappy with the product for any reason, simply call or email our customer support team and return the unused portion of the product within 90 days of your order. We’ll refund every penny of your purchase (less shipping), no questions asked!

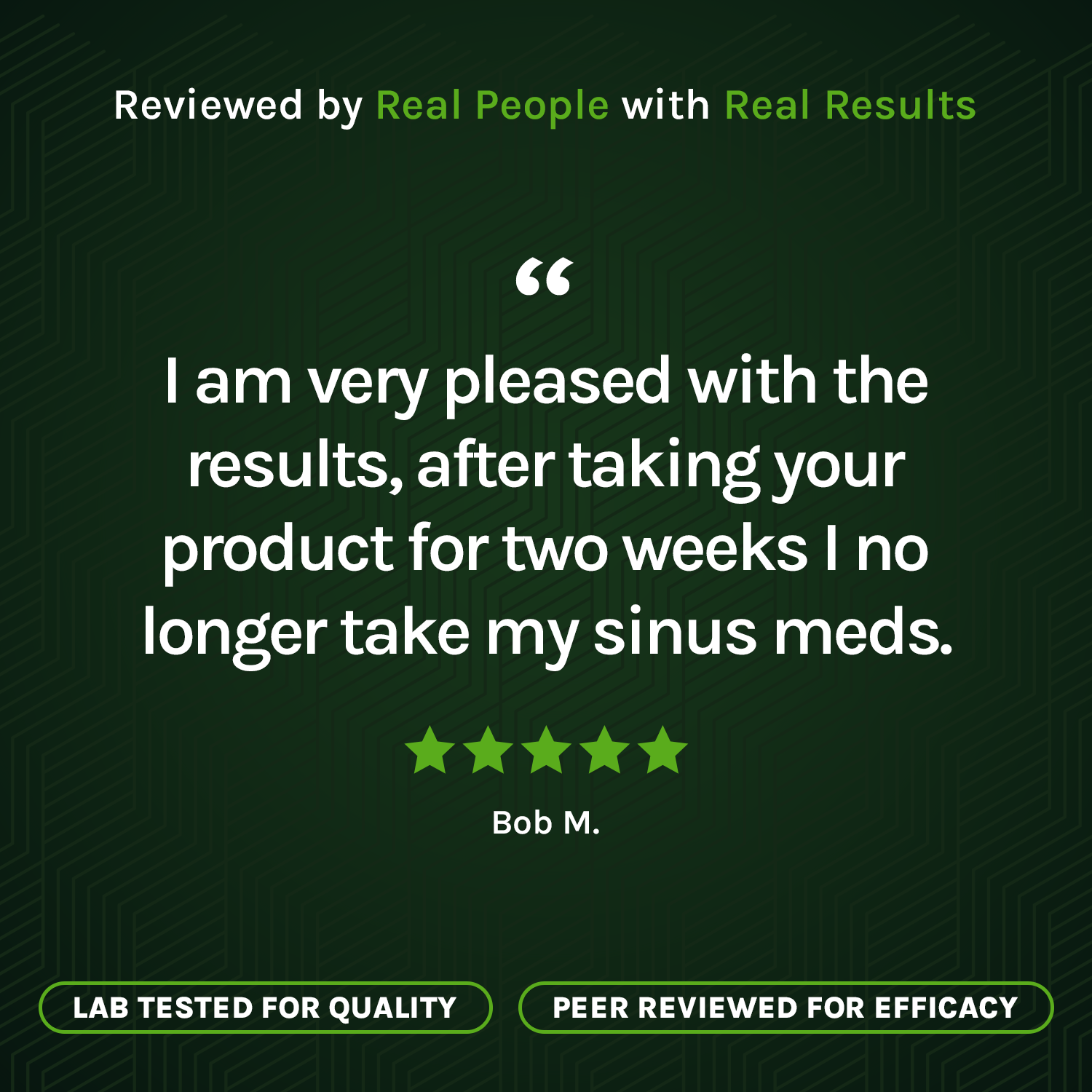
My Sinus Miracle Customer Reviews
My Sinus Miracle does work wonders
My Sinus Miracle does work wonders. my sinuses are pretty clear and breathing is easy. Sounds great to me!
LOVE the product from day 1
LOVE the product from day 1. I feel the sinus supplement has really helped me; in the beginning I took 2 a day to get my allergies "under control". I now take 1 a day most days. I have been able to minimize use of my nasal cleaner and my sprays!! VERY WORTHY product!!!!
My Sinus Miracle performed as it advertised it would
My Sinus Miracle performed as it advertised it would. Excellent customer service.